|
Condyloma (Venereal Warts) |
|
Clinical Warts Condyloma acuminata, (venereal warts) are caused by a virus known as "Human Papilloma Virus" (HPV). There are two categories of warts, clinical and subclinical. Clinical warts appear as tiny, cauliflower-like, raised lesions around the opening of the vagina or inside the vagina. These lesions appear flesh-colored or white, are not tender and have a firm to hard consistency. If they are on the outside of the vagina or vulva, they are generally symptomatic, causing itching, burning, and an uncomfortable sensation during intercourse. If they are inside the vagina, they generally cause no symptoms. |
|
|
Subclinical Warts The second category, subclinical warts, are invisible to the naked eye, are flat and colorless. They usually do not cause symptoms, although they may cause similar symptoms to the raised warts. These subclinical warts can be visualized if the skin is first soaked for 2-3 minutes with vinegar (3-4% acetic acid) and then viewed under magnification (4-10X) using a green or blue (red-free) light source. Venereal warts are not dangerous and have virtually no malignant potential. Clinical warts may be a nuisance and so are usually treated. Subclinical warts are usually not treated since they are not a nuisance (most people with subclinical warts are unaware of their presence).
|
|
Treatment Treatment consists of removal of the wart. This can be accomplished in any number of ways, some more painful than others:
|
|
|
|
Remember that in treating the warts, you are actually destroying the patient's skin which has responded in a strange and annoying way to the presence of the HPV. You are not getting rid of the HPV itself. |
|
 Vaginal wall condyloma |
Persistence of Virus HPV is a sexually-transmitted virus which usually causes no symptoms but occasionally causes warts. The virus spreads throughout the skin of the vulva and vagina (as well as the inner thighs and lower abdomen), where it disappears into the skin cells and usually remains dormant forever. Like many other viruses, if the patient's immune system allows the virus to grow, it can reappear and cause warts. This virus is extremely common, infecting as many as 1/3 of the adult, sexually-active population. There is no known way to eliminate the virus from all skin cells.
|
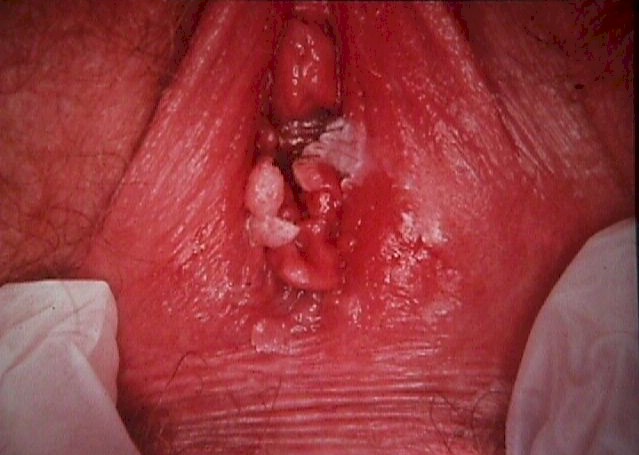
 Vulvar condyloma in a victim of child sexual abuse |
Transmission Patients with HPV are contagious to others, but there is no effective way to prevent its spread. Some physicians recommend condoms, but because the virus is found in areas of the skin beyond the condom, this is not likely to be effective. Some physicians recommend aggressive treatment of all warts, in the belief that active warts are more contagious than inactive virus within the skin. This theory has not, so far, been proven to be true. Dysplasia About 1/3 of all adult, sexually-active women have been infected with HPV, but probably less than 10% will ever develop dysplasia. Most (90%) of those with dysplasia will have mild dysplasia which will either regress back to normal or at least will never progress to a more advanced stage. Relation to Cancer Most women with moderate to severe dysplasia of the cervix, if left untreated, will ultimately develop cancer of the cervix. If treated, most of these abnormalities will revert to normal, making this form of cervical cancer largely preventable. Cervical dysplasia is usually a slowly-changing clinical problem. There is indirect evidence to suggest that on average, it takes about 10 years to advance from normal, through the various stages of dysplasia, and into cancer of the cervix. Of course, any individual may not follow these rules. In providing medical care to women with cervical dysplasia, good follow-up is important, but urgent medical evacuation is usually not indicated for less threatening categories of dysplasia. |
|
Evaluation In any patient with venereal warts (condyloma), you should look for possible dysplasia of the cervix. This is best done with colposcopy, but a simple Pap smear can be very effective. Because HPV causes warts and is also associated with dysplasia, more frequent Pap smears (every 6 months) is a wise precaution, at least initially. If dysplasia is found, gynecologic consultation will be necessary, although this may be safely postponed for weeks or months if operational requirements make consultation difficult. |

