Chest X-ray |
| Normal Chest X-ray | Reading a Chest X-ray | Pneumonia |
The Chest X-ray
is probably one of
the most commonly seen plain films, and is one of the most difficult to master.
There are many ways to evaluate the chest.
A systematic approach is usually the best.
One method is described here.
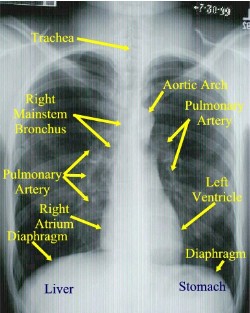

Normal Posterior to Anterior (PA) Chest X-ray
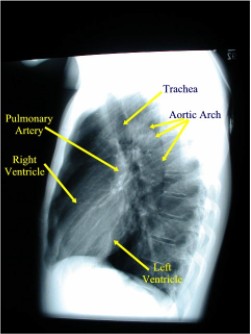
Normally a PA and Lateral View are obtained. By convention on the PA View, the x-rays enter the patient posteriorly and exit anteriorly (with the patients chest on the film cassette), therefore minimizing the cardiac magnification. On the lateral view, the patients left side is against the film, therefore the right side would be magnified.
-
Get a mental image of the patient:
-
Demographics
-
Gender
-
Size
-
Shape
-
Position of patient
-
Approximate age
-
Lines & tubes (position, course, complications)
-
Foreign bodies.
-
-
Evaluate soft tissues systematically: Don’t forget:
-
Neck
-
Shoulders
-
Diaphragm (the right diaphragm usually is 2-3 cm higher than the left)
-
Abdomen
-
Breast tissue
-
-
Evaluate the lungs (Interstitium, airways and Pleura):
-
Inflation status
-
Pleural margins
-
Abnormal densities/lucencies
-
Masses
-
Infiltrates
-
Calcifications
-
Fissure locations and thickness. The RUL Bronchus is always higher than the LUL bronchus.
-
-
Change your attention to the blood vessels:
-
The size, location and distribution (the left pulmonary artery usually is higher the left).
-
Don’t forget to check the lateral as this is the best way to look at the posterior costophrenic recess, anterior/posterior mediastinum, and help you localize lesions suspected on the frontal view.
-
-
Note the “Special Interest” and often missed areas twice:
-
Apices (esp. RUL- where most cancer lives)
-
Peripheral lung margins
-
Hilar, retrocardiac, cardiophrenic and costophrenic angles.
-
-
Focus attention now to the Mediastinum: Evaluate Size, shape, position in both views PA/LAT. Attention to the mediastinal lines
-
Heart: Check both PA/LAT views. Size, shape, and silhouette. Look for any chamber enlargement. Evaluate course of Aorta and position of arch, Pulmonary Arteries.
-
Margin of SVC (frontal View).
-
Right Paratracheal Stripe (normal is <5mm, usually 2-3mm), which terminates at the azygous vein (this portion should be 1.0cm or less). Never extends below the right bronchus.
-
Left Subclavian Stripe: Normally 1.0-1.5 cm.
-
On the lat view, the posterior tracheal wall if seen should measure no more than 4mm
-
Paraesophageal line: seen only on the PA view. (interface between right lower lobe and mediastinal edge along the esophagus/azygous vein – also called the azygoesophageal line.) It should be straight, bulging could indicate a node or mass (90% of all localized paraspinal masses are neurogenic tumors (particularly neruofibromas and ganglioneuromas.)
-
Aorticopulmonary window: Seen on frontal view formed by overlap of the Aortic arch and left pulmonary artery. Space should be clear as the left upper lobe fills in this area. It should also be concave, any bulge could signify nodes or mediastinal mass.
-
-
Bones:
-
Chest wall
-
Bony thorax including spine.
-
Look for abnormal joints, bony lytic/blastic or soft tissue lesions, and free air, etc
-
Several signs help evaluate
processes:
- Silhouette sign:
Silhouette sign is extremely
useful in localizing lung lesions.
(e.g. loss of right heart border in RML pneumonia)
- Air Bronchogram:
As the bronchial tree branches, the cartilaginous rings become thinner and
eventually disappear in respiratory bronchioles. The lumen of bronchus
contains air as well as the surrounding alveoli. Thus usually there is no
contrast to visualize bronchi.
If you see branching
radiolucent columns of air
corresponding to bronchi
, this usually means air-space (alveolar) disease. Usually one of these: blood, pus, mucous, cells, protein.
- Extra pleural sign:
Signifies Chest Wall disease. Peripheral
location with concave edges.
-
Anatomic landmarks
- Anterior & Posterior junction lines: respectively, the anterior and posterior conjunction of the right and left visceral and parietal pleural layers at the midline of the thorax.
- 2mm linear line projecting
over the trachea. Note the posterior junction line extends above the
clavicles
This section written by:
LCDR Ron Boucher, MC, USN
LT Hugh McSwain, MC, USN
With some assistance from:
Source: Operational Medicine 2001, Health Care in Military Settings, NAVMED P-5139, May 1, 2001, Bureau of Medicine and Surgery, Department of the Navy, 2300 E Street NW, Washington, D.C., 20372-5300CDR Michael Puckett, MC, USN
ENS Robert Post, MC, USNR