|
History |

|
In obstetrics and gynecology, as in most other specialties, the patient's history is of extraordinary importance. It not only provides some insight into what might be troubling the patient, but in about 90% of cases, it will provide the diagnosis. Some aspects of history-taking are the same as might be found in a general medicine practice. Others are very specific to OB-GYN complaints. Chief Complaint
In writing up your report of a visit, put the "CC" right up at the top where everyone can read it and you won't forget it. Past History
For patients not previously seen or for whom you have no medical records, you should note any previous significant medical or surgical illness, and allergies.
Medications
|
 |
OB-GYN History Some aspects of the patient's OB and GYN history are very relevant to their current situation. Among these are:
|
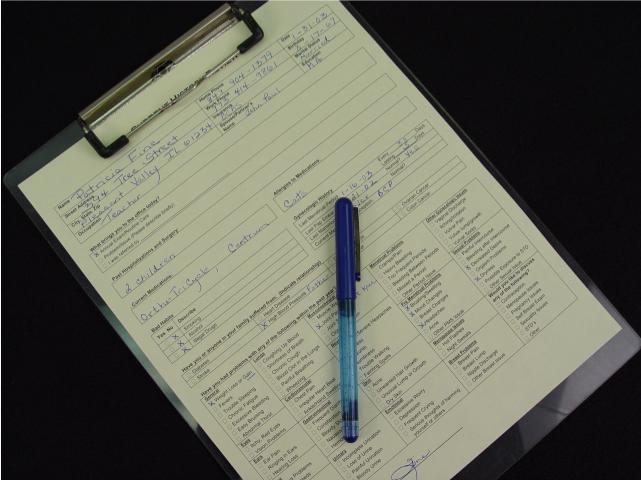 Patient Questionnaire In many practices, patients coming into the office are routinely asked to fill out a form that summarizes their Chief Complaint, Past History, Medications, and a Review of Systems. This is the form I use in my office. I like it because it gives the patient an opportunity to explain their situation in their own words (within the provided structure), and makes sure there is nothing worrying the patient that I might have overlooked. |
Menstrual History
Pregnancy History
Contraception
If she answers, "none" to this question, I always wonder why that might be. Perhaps:
|
 |
Sexual History The depth of your sexual history inquiries will depend on why the patient is seeing you and the clinical circumstances. For some encounters, sexual history is irrelevant and omitted. For other encounters, an abbreviated sexual history is appropriate. For some, a full and detailed sexual history is the needed. In those cases, questions may include:
For some patients (and some physicians), dealing with these issues may be stressful. Ask your questions in a direct, honest, and non-threatening way and you will usually find the patient responds similarly. |
 |
Nutrition For women with a normal, balanced diet, nutritional supplements are probably not necessary, but most people have difficulty maintaining a normal balanced diet. For those women, a daily multivitamin can be very helpful in making up for any nutritional deficiencies. Additional iron is particularly helpful for women in maintaining a positive iron balance. Otherwise, the steady loss of iron through menstruation can lead to some degree of anemia. For women anticipating a pregnancy, Folic acid 400 mg PO daily is recommended by the Center for Disease Control to reduce the risk of birth defects related to the spine. I sometimes will ask:
|

|
Exercise Women who exercise regularly will generally experience less trouble with cardiovascular disease, bone loss (osteoporosis), weight control, and depression. To be most effective, the exercise should be strenuous enough to cause sweating, last at least 20 minutes, and occur several times a week. Lesser amounts of exercise may also be beneficial.
As a group, women are more likely than men to sustain minor athletic injuries when exposed to the same degree of athletic stressors. Reasons for these findings may include level of training or fitness, degree of experience with exercise, architectural construction of the pelvis and lower limbs, and possibly hormonal effects. I advise women to try to avoid athletic injuries while continuing to exercise by not performing the same exercise two days in a row. This gives their body 48 hours to recover. |
|
Mood Depression is diagnosed whenever a depressed mood or loss of interest/pleasure is associated with at least four other symptoms, consistently over a two-week period. (DSM-IV)
|
|
|
Intimate Partner Abuse Physical abuse of intimate partners is much more common than most people believe. 8% of women will report of history of such violence, while 29% will report such a history, if asked. IPA encompasses child abuse, elder abuse, and both male and female partner physical abuse. |