|
Electronic Fetal Heart Monitoring |
  Electronic fetal monitors continuously record the instantaneous fetal heart rate on the
upper channel and uterine contractions on the lower channel. They do this by attaching,
either externally (and non-invasively) or internally, to detect the fetal heart and each
uterine contraction. Electronic fetal monitors continuously record the instantaneous fetal heart rate on the
upper channel and uterine contractions on the lower channel. They do this by attaching,
either externally (and non-invasively) or internally, to detect the fetal heart and each
uterine contraction.Listen to a normal fetal heart beat Labor is an inherently dangerous life event for a fetus and its mother. In the majority of cases, everything goes smoothly enough and ends happily. In a minority of cases, there are some problems. Electronic fetal monitoring is used to provide:
Originally, electronic fetal monitoring was thought to be able to prevent such newborn problems as stillbirth, brain damage, seizure disorders, and cerebral palsy. This hope proved to be overly optimistic. Unfortunately, and contrary to earlier thinking, most of the problems that lead to stillbirth, brain damage, seizure disorders and cerebral palsy are not intrapartum problems, but have already occurred by the time a patient comes in to labor and delivery. Nonetheless, electronic fetal monitoring has proved so useful in so many ways that it has become a prominent feature of intrapartum care, and indispensable for high risk patients. Two forms of continuous electronic fetal heart monitoring are used, internal and external. Internal monitoring provides the most accurate information, but requires a scalp electrode be attached to the fetus, and a pressure-sensing catheter to be inserted inside the uterine cavity. Both of these require membranes be ruptured and both have small, but not inconsequential risks. For that reason, they are usually used only when the clinical circumstances justify the small increased risk of complication. External monitoring usually provides very good information about the timing of contractions and the fetal response. External monitoring consists of belts worn by the mother during labor that record the abdominal tension (indirectly recording a contraction), and the instantaneous fetal heart rate. External monitoring has the advantages of simplicity, safety, availability, and reasonable reliability under most general obstetrical circumstances. However, it is subject to more artifact than internal monitoring, may not detect subtle changes, and may not accurately record the information, particularly if the mother is overweight or active.
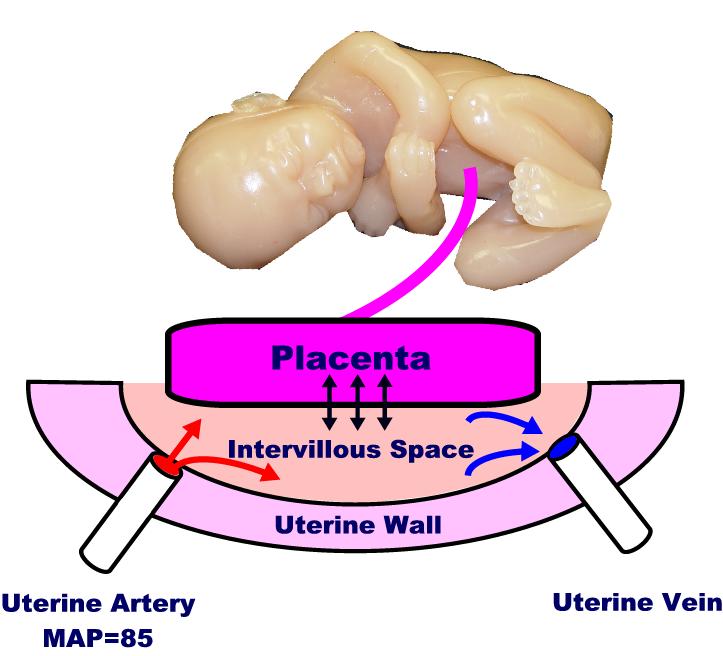
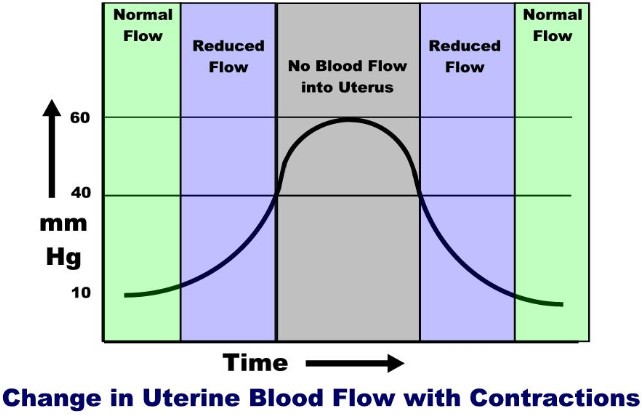
Uterine Blood Flow The placenta floats on top of the IVS, with its chorionic villi dipping down into the pool. Across the villous membrane pass oxygen, carbon dioxide, nutrients and waste products. Some of this passage is active transport (eg, glucose), some facilitated (eg, because of pH gradient), and some is passive. Many factors influence uterine blood flow delivery to the IVS, including:
Once the maternal blood reaches the IVS, oxygen and nutrients must still must traverse the villous membrane. If thickened (as with edema or infection), then transvillous transport of materials will be impaired, at least to some degree. Listen to the Doppler sound of maternal blood flowing through the uterine artery
Baseline Fetal Heart Rate
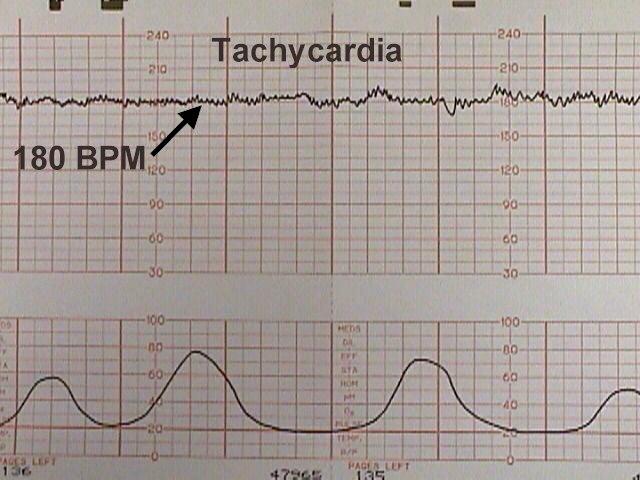
It can also increase in the presence of more worrisome problems, including:
Most tachycardias are not indicative of fetal jeopardy, particularly in the absence of any other FHR abnormalities.
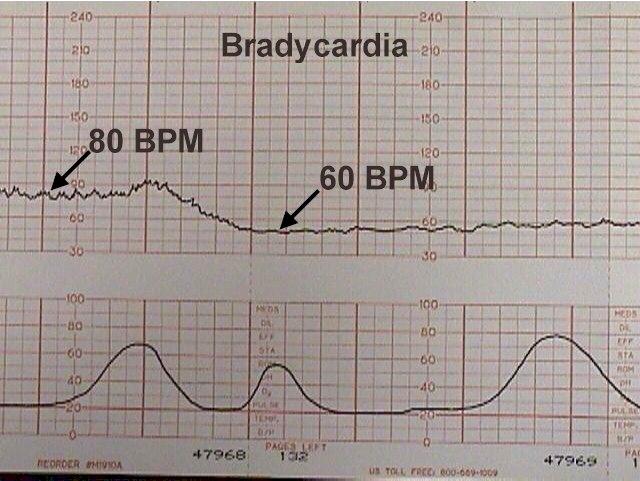
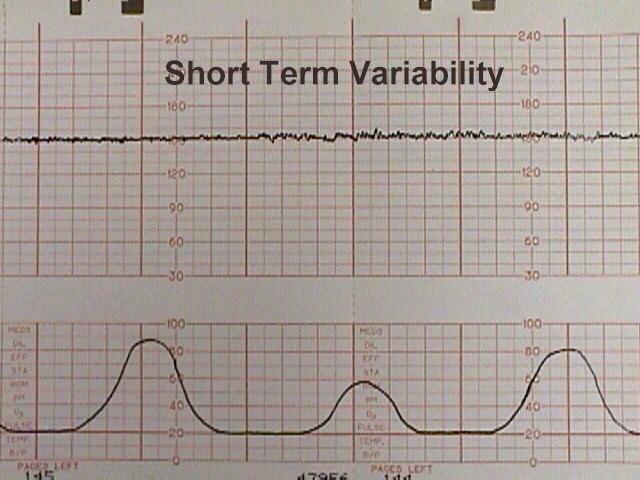
Mild bradycardia (to 80 or 90 BPM) with retention of beat-to-beat variability is common during the second stage of labor and not of great concern so long as delivery occurs relatively soon. Moderate to severe bradycardia (below 80 BPM) with loss of beat-to-beat variability, particularly in association with late decelerations, is more troubling and may indicate fetal distress, requiring prompt resolution. Variability
Reduced variability may also occur:
Persistent or progressively reduced variability is not, by itself, a sign of fetal jeopardy. But in combination with other abnormalities may indicate fetal intolerance of labor.
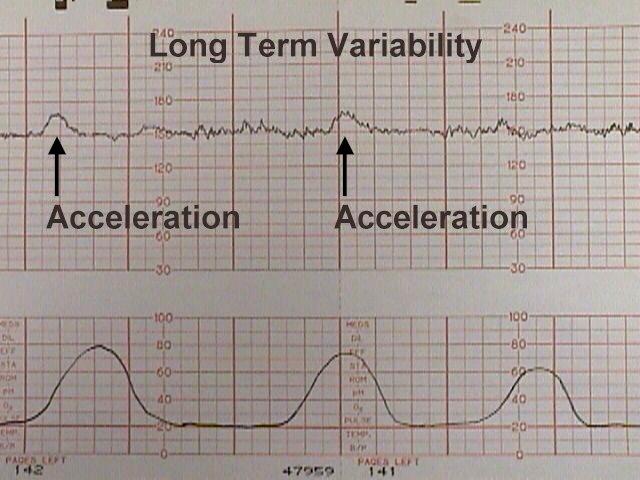
During labor, no significance is attached to the absence of fetal accelerations.
Effect of Contractions
Maternal mean arterial pressure (MAP) is around 85 mm Hg. The pressure on the inside of the uterus (at rest) is around 10 mm Hg. The pressure within the uterine muscle (intramyometrial pressure or IMP) is usually about 2-3 times that of the intra-amniotic pressure. Because of these pressures, blood flows from the high pressure uterine arteries, through the intramyometrial spiral arteries (and past the medium pressure intramyometrial zone) and into the low pressure intravillous space. From the IVS, blood is drained out through the even lower pressure venous system and returned to the mother's circulation. During a contraction, the intramyometrial pressures rise with the increased muscle tone. As the compressive pressure rises, blood flow through the spiral arteries diminishes (less pressure gradient to drive the blood through them), and then stops when the IMP equals the MAP. The IMP usually equals the MAP when the amniotic fluid pressure is around 40 mm Hg. (Remember that the intramyometrial pressure is 2-3 time that of the amniotic fluid pressure). As the contraction eases up, blood flow through the spiral arteries resumes and by the end of the contraction, blood flow is back to normal. Thus, with each contraction of any significance, there is initially reduced blood flow to the intervillous space, then a cessastion of blood flow, followed by a gradual resumption of blood flow. On one level, you could imagine the danger of the fetal oxygen supply being interrupted by each uterine contraction. On another level is the realization that for a normal fetus, this interruption is nearly trivial (similar to holding your breath for 5 seconds). But if the contractions are coming too frequently (with very little time between contractions for the fetus to resupply), or if the fetus already has a significant problem, then contractions can pose a threat. Contraction Patterns A normal contraction pattern in active labor shows contractions occurring about every 2-3 minutes and lasting about 60 seconds.
Coupling If labor is progressing normally, coupling can be ignored. Often, however, coupling is associated with dysfunctional progress in labor. In these cases, coupling can be treated with:
Tachysystole Tachysystole is most often caused by too much oxytocin stimulation. In these cases, the simplest solution is to reduce or stop the oxytocin to achieve a more normal and better tolerated labor pattern. Other causes of tachysystole include:
In cases of spontaneous tachysystole, increasing maternal hydration and placement in the lateral decubitus position may slow the contractions.
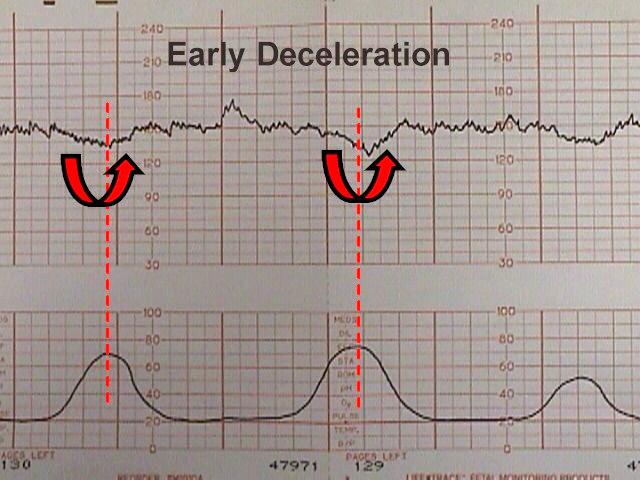
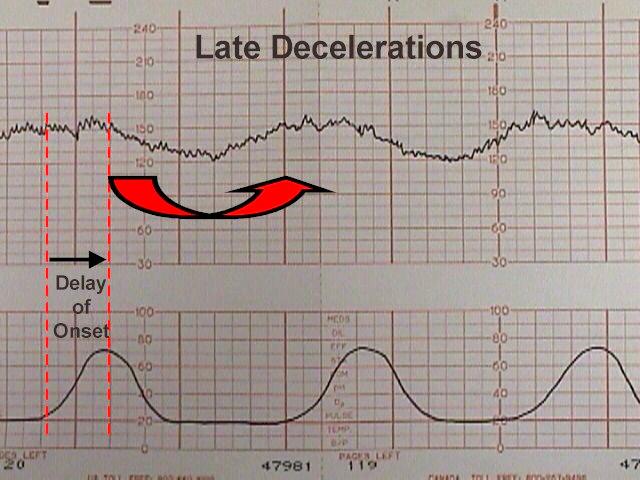
Periodic Heart Rate Changes
Each has its own features and clinical significance. In addition, a fetus may demonstrate combined decelerations (for example, a severe variable deceleration with a late deceleration component.)
These innocent changes are thought to be due, in many cases, to fetal head compression within the birth canal. Sometimes, patients demonstrating early decelerations will later develop variable decelerations (see below). Late decelerations
Clinically, the development of late decelerations is a worrisome sign that the fetus has very little reserve. Techniques that may be used to correct this problem include:
If the late decelerations are persistent and non-remediable, this is considered "fetal distress," "fetal intolerance of labor," or a "non-reassuring fetal heart rate pattern." Such patients should be delivered promptly to avoid fetal injury or death. Sometimes cesarean section is required to achieve prompt delivery. If persistent and not correctable, they represent a threat to fetal well-being.
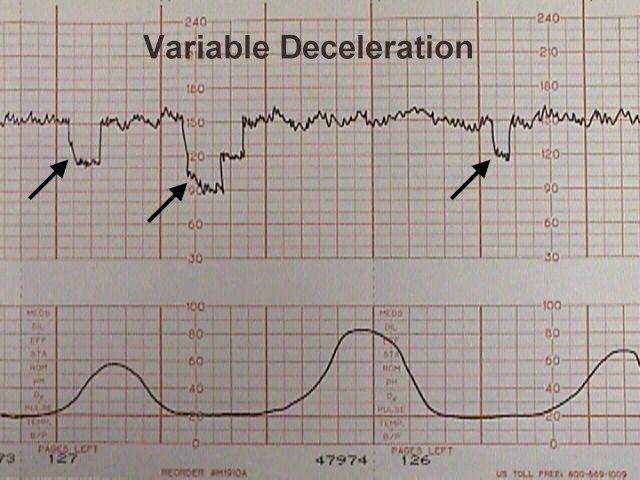
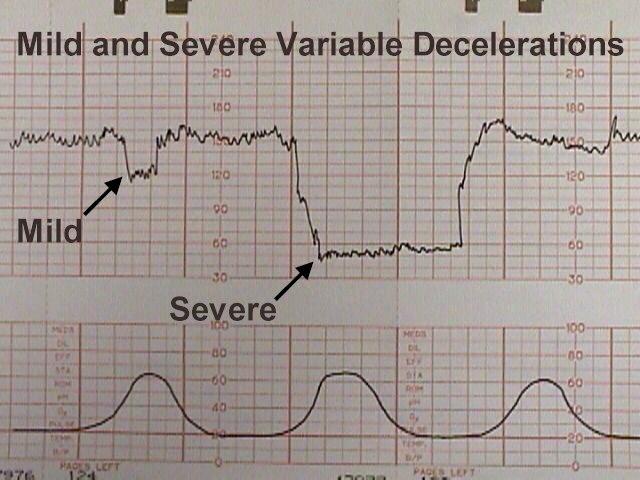
Variable Decelerations Typically, they have an abrupt onset and rapid recovery (in contrast to other types of decelerations which gradually slow and gradually recover. Variable decelerations are thought to represent a vagal response to some degree of umbilical cord compression. If the umbilical cord is only slightly compressed, this will obstruct the umbilical vein (low pressure system) which returns re-oxygenated blood to the fetal heart. The initial normal fetal response to this is a slight increase in fetal heart rate to compensate for the lack of blood return and the slowly diminishing oxygen supplies. If this slight increase in FHR is followed by a major drop in FHR, this phenomenon is called a "shoulder." As pressure on the umbilical cord increases, the high-pressure umbilical arteries become occluded. When this happens, there is an immediate rise in fetal blood pressure. 30% of the fetal cardiac output goes to the placenta and if that flow is blocked, the fetus will rapidly develop significant hypertension. The normal fetus will respond to this hypertension by immediately slowing the heart down by sending a signal through the vagus nerve. When the umbilical cord obstruction is released, the vagal response disappears and the fetal heart returns to normal. If a mild degree of cord compression continues (enough to continue to obstruct the umbilical veins for a while), then another "shoulder" may appear at the end of the deceleration. If the variable deceleration lasts long enough to cause hypoxia, there may be a more gradual rise back to the baseline and some "overshoot." Overshoot means the heart rate goes higher than the baseline for a while, to compensate for the mild degree of hypoxia and acidosis that has occurred during that deceleration. If you exercise vigorously for a minute, your muscle tissues will acquire some degree of oxygen debt and a mild degree of local acidosis. When you sit down and rest, your heart rate will be higher than before you started exercising, but will return to normal as you resupply your muscles with oxygen and remove the local waste products. The fetus responds in a similar fashion. Variable decelerations, unlike late decelerations, are not caused by hypoxia, although if severe enough, frequent enough and persistent enough, can ultimately lead to some degree of fetal acidosis. The interventions to effectively treat variable decelerations may include:
Occasional mild or moderate variable decelerations are common and not considered threatening. They are seen in the majority of laboring patients at some time or other. They are more common in the second stage of labor. Mild variable decelerations do not dip below 70 BPM and last less than 30 seconds. Severe variable decelerations dip below 60 BPM for at least 60 seconds ("60 x 60"). If persistent and not correctable by simple means, they can be threatening to fetal well-being. Like persistent, non-remediable late decelerations, fetuses demonstrating persistent, non-remediable severe variable decelerations should be delivered promptly, preferably vaginally, but by cesarean section if necessary.
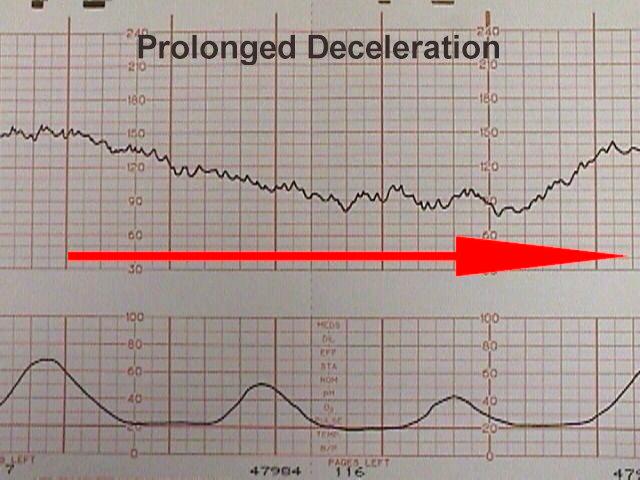
Some of these are largely self-correcting, such as the deceleration following paracervical block, while others (maternal supine hypotension) respond to simple measures such as repositioning. Other causes (such as umbilical cord prolapse) require prompt intervention to avoid or reduce the risk of fetal injury. |