|
Initial Evaluation in Labor |
 Most labors and deliveries are safe, spontaneous processes, requiring little or no
intervention, and result in a healthy mother and healthy baby. Some are not so safe and
may not have the same good outcome. The two purposes of L&D management are:
Most labors and deliveries are safe, spontaneous processes, requiring little or no
intervention, and result in a healthy mother and healthy baby. Some are not so safe and
may not have the same good outcome. The two purposes of L&D management are:
- Monitoring the mother and baby for abnormalities which, through detection and treatment, will lead to a happy outcome for both.
- Applying knowledge and skills to improve on the quality of the experience or outcome which nature would otherwise provide. This would include such areas as pain relief, prevention or repair of lacerations, reducing fatigue, anemia, risk of infection, and injury to the mother and baby.
Initial Evaluation of a Woman in Labor
An initial evaluation is performed to:
- Evaluate the current health status of the mother and baby,
- Identify risk factors which could influence the course or management of labor, and
- Determine the labor status of the mother.
History
Interview the patient as soon as she arrives.
Certain key questions will provide considerable insight into the patient's pregnancy and current status:
- What brought you in to see me?
- Are you contracting? When did they start?
- Are you having any pain?
- Are you leaking any fluid or blood? When did that begin?
- Have there been any problems with your pregnancy?
- Has the baby been moving normally?
- When did you last eat? What did you have?
- Are you allergic to any medication?
- Do you normally take any medication?
- Have you ever been hospitalized for any reason?
Use a form that covers the prenatal history and risk assessment
Risk Factors
For some women, there is a greater chance of problems during labor than for other
women. Various factors have been identified to try to predict those women who will
experience problems and those who will not. These are called risk factors. Some are more
significant than others. While most women with any of these factors will experience good
outcomes, they may benefit from increased surveillance or additional resources.
|
Moderate increase in risk |
More than moderate increase in risk |
|
|
 |
Vital Signs
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Feel with your hand for contractions, when the uterus becomes hard and rises up out of the abdomen. |
Contractions In some cases, the patient will have been timing the contractions. Placing your hand on the maternal abdomen, you will be able to feel each contraction as the normally soft uterus becomes firm and rises out of the abdomen. Time the contractions from the beginning of one to the beginning of the next one. Also note the duration of the contractions and their relative intensity (mild, mild-to-moderate, moderate, severe). Contractions can also be followed by use of an electronic fetal monitor. In this case, the paper channel will show the rhythmic peaks that correspond to a uterine contraction. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Listen for the fetal heartbeat |
Fetal Heart Rate This can be done with a fetal Doppler device, and electronic fetal monitor, ultrasound visualization of the fetal heart, or a DeLee type stethoscope. Normal rates are between 120 and 160 BPM at full term. Post term babies may sometimes normally have rates as low as 110 BPM. The fetal heart rhythm should be regular, without any skipped beats or compensatory pauses. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
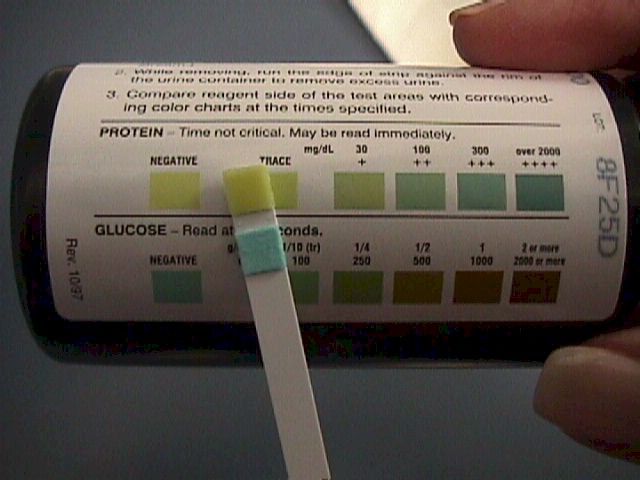 |
Urine for Protein and Glucose Check the urine for protein and glucose. The presence of protein (1+ or greater) can suggest the presence of pre-eclampsia. This level of 1+ on a random urine sample corresponds to about a:
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

|
Estimated Fetal Weight Estimate the fetal weight. An average baby at full term weighs 7 to 7 1/2 pounds. By feeling the maternal abdomen, an experienced examiner can often predict within a pound the actual birthweight. A woman who has delivered a baby in the past can often do about as well in predicting her current baby's weight if you ask her, "Is this baby bigger or smaller than your last?"
Significant landmarks are:
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
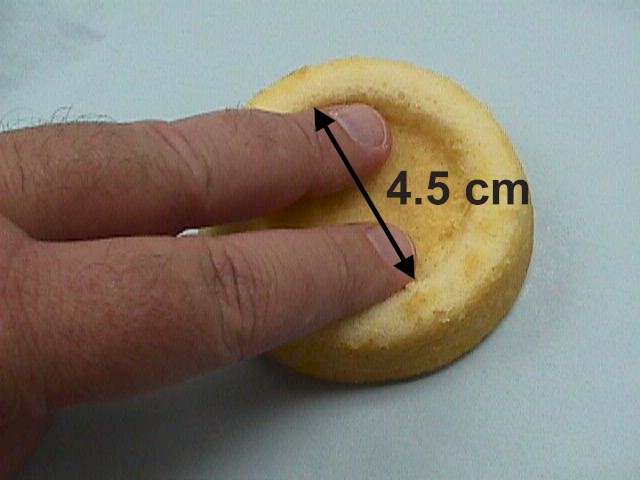 |
Cervical Dilatation and Effacement Using sterile gloves and lubricant, perform a vaginal exam and determine the dilatation and effacement of the cervix. A small amount of bleeding during the days or hours leading up to the onset of labor is common and called "bloody show." Dilatation is expressed in centimeters. I have relatively large fingers, and for my hands, I make the following generalizations:
Effacement is easiest to measure in terms of centimeters of thickness, ie., 1 cm thick, 1.5 cm thick, etc. Alternatively, you may express the thickness in percent of an uneffaced cervix...ie, 50%, 90%, etc. This expression presumes a good knowledge of what an uneffaced cervix should feel like. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Leopold's Maneuvers are used to determine the orientation of the fetus through abdominal palpation. 1. Using two hands and compressing the maternal abdomen, a sense of fetal direction is obtained (vertical or transverse). 2. The sides of the uterus are palpated to determine the position of the fetal back and small parts. 3. The presenting part (head or butt) is palpated above the symphysis and degree of engagement determined 4. The fetal occipital prominence is determined.. |
Fetal Orientation There are basically 3 alternatives:
Most of the time, the fetus will be head first (vertex). The easiest way for a relatively inexperienced examiner to determine this presentation is by pelvic exam. The fetal head is hard and bony, while the fetal butt is soft everywhere except right over the fetal pelvic bones. When the baby is presenting butt first, the presenting part is very soft, but with hard areas within it (sacrum and ischial tuberosities). If one or both feet are presenting first, you will feel them. If you don't feel any presenting part (head or butt) on pelvic exam, there is a good chance the baby is in transverse lie (or oblique lie). Then things get a little more complicated. Transverse lie or oblique lie can be suspected if the fundal height measurement is less than expected and if on abdominal exam, the basic orientation of the fetus is side-to-side. More experienced examiners can tell much from an abdominal exam. Making a "V" with their thumb and index finger and pressing down just above the pubic bone, they can usually feel the hard fetal head at the pelvic inlet.
Evaluation of the Maternal Pelvis Techniques to evaluate the maternal pelvis are found here. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Positive Nitrazine Test for Amniotic Fluid |
Status of Fetal Membranes A history of a sudden gush of fluid is suggestive, but not convincing evidence of ruptured membranes. Sudden, involuntary loss of urine is a common event in late pregnancy. Usually, ruptured membranes are confirmed by a continuing, steady leakage of amniotic fluid, pooling of clear, Nitrazine positive fluid in the vagina on speculum exam. Vaginal secretions are normally slightly acid, turning Nitrazine paper yellow. Amniotic fluid, in contrast, is a weak base, and will turn the Nitrazine paper a dark blue. Dried amniotic fluid forms crystals (ferning) on a microscope slide. Vaginal secretions do not. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
Blood Count Women with significant anemia are more likely to have problems sustaining adequate uterine perfusion during labor. They also have less tolerance for hemorrhage than those with normal blood counts. Women with no prenatal care should, in addition, have a blood type, Rh factor, and atypical antibody screen performed. Other tests may be indicated, based on individual history. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||





