|
3rd Trimester Bleeding |
 Bloody Show |
Bleeding during the third trimester has special clinical significance, encompassing problems that are quite serious and those that are normal or expected. It is important to be able to distinguish between them.
As the cervix thins (effaces) and begins to dilate in preparation for labor, the patient may notice the passage of some bloody mucous. This is a normal event during the days leading up to the onset of labor at term. If this is the only symptom, the patient can be reassured of its normalcy. If the patient is also having significant contractions, she should be evaluated for the possible onset of labor.
If this bloody mucous show appears prior to full term, then it may signal the imminent onset of preterm labor. These patients are evaluated for possible pre-term labor.
Read more about the evaluation and management of pre-term labor.
Bleeding that is more than bloody mucous (bright red, no mucous, passage of clots) requires further evaluation.
Cervicitis and cervical
trauma
During pregnancy, the cervix becomes softer, more fragile, and
more vulnerable to the effects of trauma and microbes.
Cervical ectropion, in which the soft, mucous-producing endocervical mucosa grows out onto the exocervix is common among pregnant women. This friable endocervical epithelium bleeds easily when touched. This situation can lead to spotting after intercourse, a vaginal examination, or placement of a vaginal speculum.
Cervical ectropion also can lead to cervicitis. The normal squamous cell cervical epithelium is relatively resistant to bacterial attack. The endocervical mucosa is less resistant. If infected, the cervical ectropion is even more likely to bleed if touched.
These changes are usually easily seen during a vaginal speculum exam.
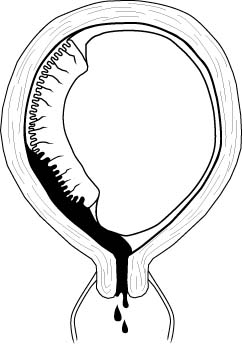 |
Placental abruption is also known as a premature separation of the placenta. All placentas normally detach from the uterus shortly after delivery of the baby. If any portion of the placenta detaches prior to birth of the baby, this is called a placental abruption. Placental abruption occurs in about 1% of all pregnancies.
A placental abruption may be partial or complete.
A complete abruption is a disastrous event. The fetus will die within 15-20 minutes. The mother will die soon afterward, from either blood loss or the coagulation disorder which often occurs. Women with complete placental abruptions are generally desperately ill with severe abdominal pain, shock, hemorrhage, a rigid and unrelaxing uterus.
Partial placental abruptions may range from insignificant to the striking abnormalities seen in complete abruptions.
Clinically, an abruption presents after 20 weeks gestation with abdominal cramping, uterine tenderness, contractions, and usually some vaginal bleeding. Occasionally, the blood loss is trapped inside the uterus. These cases are called "concealed abruptions."
A number of factors are associated with an increased risk of placental abruption, among them:
|
|
Abruptions are often diagnosed clinically, based on the symptoms of bright red vaginal bleeding, frequent contractions and uterine tenderness. There are no laboratory findings that are specific for placental abruption. In mild cases, laboratory tests are usually normal. In more advanced cases, the Hgb and Hct go down, as do the platelets and fibrinogen (due to the massive bleeding and consumption of coagulation factors) while fibrin split products go up. Large numbers of fetal RBCs may be identified in the maternal blood.
In the case of large abruptions, ultrasound may identify a retroplacental blood clot. In milder cases, ultrasound scans are frequently normal.
Mild abruptions may resolve with bedrest and observation, but the moderate to severe abruptions generally result in rapid labor and delivery of the baby. If fetal distress is present (and it sometime is), rapid cesarean section may be needed.
Because so many coagulation factors are consumed with the internal hemorrhage, coagulopathy is common. This means that even after delivery, the patient may continue to bleed because she can no longer effectively clot. In a hospital setting, this can be treated with infusions of platelets, fresh frozen plasma and cryoprecipitate. If these products are unavailable, fresh whole blood transfusion will give good results.
|
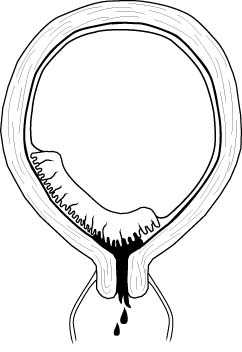
Normally, the placenta is attached to the uterus in an area remote from the cervix. Sometimes, the placenta is located in such a way that it covers the cervix. This is called a placenta previa.
There are degrees of placenta previa:
A complete placenta previa means the entire cervix is covered. This positioning makes it impossible for the fetus to pass through the birth canal without causing maternal hemorrhage. This situation can only be resolved through cesarean section.
A marginal placenta previa means that only the margin or edge of the placenta is covering the cervix. In this condition, it may be possible to achieve a vaginal delivery if the maternal bleeding is not too great and the fetal head exerts enough pressure on the placenta to push it out of the way and tamponade bleeding which may occur.
Clinically, these patients present after 20 weeks with painless vaginal bleeding, usually mild. This is in contrast to patients with placental abruption, who usually experience significant pain and contractions. An old rule of thumb is that the first bleed from a placenta previa is not very heavy. For this reason, the first bleed is sometimes called a "sentinel bleed."
Later episodes of bleeding can be very substantial and very dangerous. This can lead to hypovolemic shock and maternal death. Because a pelvic exam may provoke further bleeding it is important to avoid a vaginal or rectal examination in pregnant women during the second half of their pregnancy unless you are certain there is no placenta previa.
Factors associated with an increased risk of placenta previa include:
|
|
The location of the placenta is best established by ultrasound. If ultrasound is not available, one reliable clinical method of ruling out placenta previa is to check for fetal head engagement just above the pubic symphysis.
 Using
a thumb and forefinger and pressing into the maternal abdomen, the fetal head
can be palpated. If it is deeply engaged in the pelvis, it is basically
impossible for a placenta previa to be present because there is not enough
room in the birth canal for both the fetal head and a placenta previa. An
x-ray of the pelvis (pelvimetry) can likewise rule out a placenta previa, but
only if the fetal head is deeply engaged. Otherwise, an x-ray will usually not
show the location of the placenta.
Using
a thumb and forefinger and pressing into the maternal abdomen, the fetal head
can be palpated. If it is deeply engaged in the pelvis, it is basically
impossible for a placenta previa to be present because there is not enough
room in the birth canal for both the fetal head and a placenta previa. An
x-ray of the pelvis (pelvimetry) can likewise rule out a placenta previa, but
only if the fetal head is deeply engaged. Otherwise, an x-ray will usually not
show the location of the placenta.
The clinical approach depends on the clinical situation. For example:
- A 3rd trimester patient who is hemorrhaging (500 cc with continuing active bleed) bright red blood should go directly to the operating room for a cesarean section to deliver her from the placental abruption or placenta previa. While en route to the OR, call for blood transfusions and labs to determine coagulopathy.
- A patient at term with regular contractions and a small amount of bloody mucous can be examined vaginally after confirming (through ultrasound or clinical exam of the abdomen) that there is no placenta previa.
- Patients with bright red vaginal bleeding that is less than hemorrhage should be carefully evaluated prior to performing a pelvic exam. Ultrasound can be helpful in locating the placenta and looking for retroplacental blood clot. Laboratory tests for coagulopathy can be helpful. Hgb is useful, not to determine whether to transfuse or not (that is a clinical, not laboratory decision), but to indicate the margin of safety available to the clinician in caring for this patient. Continuous electronic fetal monitoring is important to determine the degree of tolerance the fetus has for this bleeding and the extent to which uteroplacental circulation has been disrupted. After ruling out a placenta previa, examine the patient with a speculum to determine the source of the bleeding (from the cervical os? from the surface of the cervix? from a laceration of the vaginal wall? etc.)
Shock is the generalized inadequate perfusion of the tissues of the body. The cause of shock may be low cardiac output (cardiogenic shock), low blood volume (hypovolemic shock), or other other etiologies (septic shock, toxic shock).
The greater the blood loss, the worse the clinical problem and the more dramatic the clinical findings. This has led to a number of systems to categorize hemorrhage according to its severity. One such system is shown here:
| Class I | Class II | Class III | Class IV | |
| Severity | Compensated | Mild | Moderate | Severe |
| % Loss | Up to 15% | 15-30% | 30-40% | >40% |
| Volume Loss | Up to 500 ml | 750-1500 ml | 1500-2000 | >2000 |
| Pulse | <100 | >100 | >120 | >140 |
| BP | Normal | Orthostatic change | Mod. Decrease | Frank Hypotension |
| Respiratory Rate | Normal | Mild increase | Tachypnea | Marked tachypnea, Respiratory failure |
| Urine (ml/hour) | >30 | 20-30 | 5-20 | None |
| Symptoms | Normal | Agitated, anxious | Confused, disoriented | Lethargic, unresponsive, Skin cold and clammy |
In real patients, there is often some overlap between classes, and not all individuals within a class will show all of these signs and symptoms.
Pregnancy itself can be a complicating factor. Following a normal vaginal or cesarean delivery, maternal blood loss may average as much as 1,000 ml, or about 20% of the maternal blood volume. In a non-pregnant adult, such a loss would likely provoke signs and symptoms of shock. But in pregnant women, this loss is tolerated, often without any significant symptoms, primarily because the mother's blood volume needs immediately after delivery are significantly less than just before delivery. The fetus and placenta (with all their metabolic needs) are gone from the mother. The uterus is firmly contracted, reducing blood flow through it and the eliminating the shunting effect of the intervillous space. The maternal peripheral blood flow, previously widely dilated, vasoconstricts, reducing the distensibility of her cardiovascular system. Her pre-preganancy blood volume has increased by about 50% over the course of pregnancy(30% increase in red cell mass) and so the loss of 20% of her blood volume during delivery is generally tolerated very well. Blood loss in excess of the normal loss, however, can be problematic, as can any significant blood loss while she remains pregnant. Unfortunately, the bleeding associated with placenta previa and placental abruption both occur while she continues to have strong metabolic needs of the fetus and placenta, significant cardiac output directed to the uterus, and significant shunting through the intervillous space.
Management of hemorrhagic shock involves two processes, recognition and treatment.
Recognition requires being alert to the significance of any observed bleeding and its context. Rapid loss of 500 cc of bright red blood during a normal vaginal delivery would not attract clinical attention, so long as it stopped as soon as the uterus firmly contracted. The same 500 cc loss from a woman not in labor would constitute hemorrhage. The sudden appearance of 500 cc of bright red blood and clots in a woman in active labor at 6 cm suggests both hemorrhage and a placental abruption.
Recognition is complicated by some of the routine procedures used during labor. Many patients receive IV fluids during labor that may partially compensate for active bleeding. It is not unusual for a woman who is steadily bleeding, but who is receiving IV fluids, to have reasonably normal vital signs up until she experiences cardiovascular collapse.
Recognition involves watching maternal vital signs for the classical signs of tachycardia, tachypnea, hypotension and oliguria, as well as the symptoms of agitation, anxiety, confusion, disorientation and lethargy. The second part of recognition is observing significant blood loss, either at an unusual time, or in excess of the expected. Either may trigger treatment for hemorrhage.
Treatment:
- IV crystalloid. Up to two liters can effectively treat mild degrees of hemorrhage. In more severe hemorrhage, it can stabilize the patient long enough to get blood transfusions going. Some physicians prefer a colloid solution (and there are arguments both for and against this). Either should be effective in helping expand the intravascular volume.
- Oxygen. This won't help a lot because the hemoglobin is already nearly 100% saturated with oxygen, but it helps enough that it is worth doing.
- Blood. The problem with shock is that not enough oxygen is getting to the tissues. Expanding the blood volume with crystalloid won't create any more red blood cells to carry oxygen to the tissues. In cases of moderate to severe shock, blood transfusions are needed.
- Trendelenberg position. If blood is not immediately available, placing the patient in a head-down position (ie, legs up in the air, or Trendellenberg position) will make available 250 to 500 cc of blood that had been pooled in the lower extremeties.
- Stop the bleeding. Do whatever needs to be done to stop the bleeding. There is an old medical expression: "All bleeding eventually stops." That's true.
Read more about the treatment of hemorrhagic shock in Emergency War Surgery
Blood transfusionThe ideal material for use in hemorrhagic shock would be disease-free, body-temperature, fresh, whole blood, with identical blood type and major and minor blood groups. This has excellent oxygen-carrying capacity, platelets, coagulation factors, volume and colloid, and would be totally non-reactive within the victim's bloodstream. Unfortunately, this ideal material does not exist (at least not when quickly needed), so we usually compromise, using various blood products, depending on the needs of the patient.
In an extreme emergency, you can give the patient type O negative packed RBCs from the blood bank. For someone whose blood type is unknown and there is no time for cross-matching, this is the best approach. If type O negative blood is not available, type O positive can be substituted with good results, but there is a fair chance that the patient (if Rh negative) will become sensitized against the Rh factor. Still, that may be preferable to losing the patient because they weren't transfused quickly enough. If the patient's blood type is known, you can give type specific blood to her. If she is type B positive, you can give type B positive blood to her. In either case, it is best to draw a plain tube of blood just before giving the non-crossmatched blood to help in figuring out her native blood type.
If you have more time, it is better to give cross-matched blood. Cross-matched means the type (A, B, AB, or O) will match, and the major factors (Rh, Kell, etc.) will match. There will undoubtedly be some minor factors that do not match, and the degree of a match hinges, in part, on the size of your blood bank and the available time.
Transfusions are usually with packed RBCs (following removal of much of the serum, coagulation factors, platelets and fibrinogen). This works well enough and is very effective at restoring oxygen carrying capacity. Give enough units so the kidney function is normal (>30 cc/hour) and the patient has no more than mild symptoms of hypovolemia. There is no specific hemoglobin concentration that should be a target. The old target of 10 gm dL of hemoglobin is too conservative, requiring more blood transfusions than are really needed.
Following transfusion, the per-unit risk of developing:
- Hepatitis C is about 1 in 3300
- Hepatitis B is about 1 in 200,000
- HIV is about 1 in 500,000
In some cases of severe hemorrhage, a coagulopathy develops as a consequence of loss of platelets and/or clotting factors. This situation can be determined through lab tests (PT, PTT, fibrinogen, platelet count, bleeding time, and others), or clinically by observing multiple bleeding sites from the mouth, gums, needle puncture sites or surgical sites. A crude estimate may be obtained by taping a red-top tube of blood to the wall. A clot should form within about 5 minutes. If it doesn't, a coagulopathy of some form can be presumed. Coagulopathy can be suspected in anyone with massive blood loss (requiring 4 or more units of RBCs to correct).
Fresh frozen plasma (FFP) contains plasma proteins and clotting factors. For patients who are actively bleeding and have a demonstrated coagulopathy with prolonged PT and PTT, FFP will help restore hemostasis. For those not actively bleeding, FFP is not often needed if the PT and PTT are prolonged no more than 1.5 times normal. FFP need not be given prophylactically with RBC transfusions in the absence of coagulopathy. However, if the total blood volume has been replaced in an individual, FFP is sometimes given.
If the only missing factor is fibrinogen (sometimes the case with placental abruptions and often the case with long-standing missed abortions), then cryoprecipitate can be given to replace the fibrinogen. Cryoprecipitate also contains von Willebrand's factor and is useful in treating bleeding patients with this particular deficiency.
Platelets are given if the platelet count falls below 50,000 and the patient continues to bleed. In the absence of bleeding, platelet counts between 10,000 and 50,000 are worrisome, but usually not an indication for platelet transfusion. If the platelets fall below 10,000, the patient should be transfused as the risk for CNS and GI bleeding rises significantly. Pre-operatively, those with platelet counts below 50,000 may be transfused.