|
Ectopic Pregnancy |
 Ectopic pregnancy means the pregnancy is not growing in its normal
location inside the uterus. Instead, it is growing elsewhere. 97% of the
time, the ectopic pregnancy is located in the fallopian tube (tubal
ectopic pregnancy) and the rest are found in the ovary, abdomen, cervix
or other nearby structure.
Ectopic pregnancy means the pregnancy is not growing in its normal
location inside the uterus. Instead, it is growing elsewhere. 97% of the
time, the ectopic pregnancy is located in the fallopian tube (tubal
ectopic pregnancy) and the rest are found in the ovary, abdomen, cervix
or other nearby structure.Incidence
The incidence of ectopic pregnancy varies with the population but is
about one in every hundred pregnancies. The incidence is higher among
women with previous tubal disease, tubal surgery, previous ectopic
pregnancy, assisted reproduction, and current IUD users. Many very early
ectopic pregnancies resolve spontaneously, so if you aggressively search
for them early in pregnancy, you will find more of them.
Ectopic
Pregnancies of Special Clinical Interest
Certain types of ectopic pregnancy carry special significance. Among
these are:
- Implantation in the distal half of the fallopian tube. This represents the vast majority of all ectopics and is the type most likely to resolve spontaneously through "tubal abortion." The closer the ectopic is to the fimbriated end, the more likely it will be to outgrow its blood supply and be expelled out the end of the tube.
- Isthmic ectopic. The isthmus is the narrowest portion of the tube, least distensible, and ectopics that grow here are more likely to rupture, and to rupture early in the course of the pregnancy.
- Cornual ectopic. These ectopics grow in the portion of the tube that passes through the uterine cornua. These tend to rupture early and violently, with massive abdominal hemorrhage. Many of the fatalities due to ectopic pregnancy are from cornual pregnancies.
Symptoms
For women without rupture, there may be no symptoms, other than the
usual symptoms of pregnancy (fatigue, breast tenderness, amenorrhea).
With rupture and intra-abdominal bleeding, the following symptoms may be
seen, depending on the extent of bleeding:
- Vaginal bleeding
- Abdominal pain
- Right shoulder pain (from blood irritating the undersurface of the right hemidiaphragm, stimulating the phrenic nerve and causing referred pain)
- Urge to defecate
- Dizziness, fainting
Physical Findings
In the case of unruptured ectopic pregnancies in the fallopian tube,
there may be no unusual physical findings. The uterus can be enlarged
appropriately, no masses found, and no tenderness in the pelvis. Some
patients, however, may show some of these findings:
- Pelvic mass (either from the enlarged ectopic, or from the corpus luteum cyst that accompanies many early pregnancies of all types)
- Pelvic tenderness, localized or generalized
- Abdominal distension
- Hypotension, tachycardia, tachypnea
The pregnancy test is positive.
- Serial Quantitative HCG levels often are low and do not show the normal doubling every 2 days. However, some (10-15%) ectopic pregnancies do show a normal rise, and some (10-15%) normal pregnancies don't show the normal doubling rate.
- Progesterone levels are sometimes very low (<5). Levels greater than 25 are usually seen with normal intrauterine pregnancies, but this is a generalization.
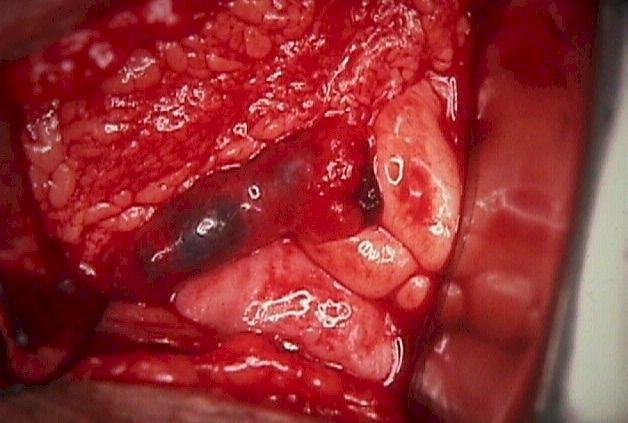
 Unruptured cornual ectopic pregnancy |
As the resolution of ultrasound has improved over the years, so has its ability to find ectopic pregnancies. It still remains true, however, that ultrasound is at its best in defining the presence of normal, intrauterine pregnancies. Some of the criteria for defining an ectopic pregnancy with ultrasound include:
- Visualization of a gestational sac, fetal pole and fetal heartbeat outside of the uterus. This is an uncommon finding with ectopic pregnancies.
- Absence of an identifiable intrauterine pregnancy when the quantitative HCG suggests it should be visible. The "discriminatory zone" is the level of HCG, above which a normal IUP is normally seen. The discriminatory zone varies from setting to setting and depends on both the skills of the operator, the resolution of the equipment, and the imaging technique (abdominal vs vaginal). Discriminatory zones range from 1,000 to 2,000 or more, depending on the clinical setting.
- Free fluid in the abdomen if there is any significant internal bleeding.
Ultrasound can be misleading at times. Occasionally, "intrauterine" pregnancies are identified that are, in fact, ectopic pregnancies with sufficient inflammatory reaction and bleeding around them to make it appear that they are surrounded by normal uterine muscle. In some other cases, an "intrauterine" pregnancy is identified that is, in fact, a "gestational pseudosac" within the uterus. This pseudosac is a response by the endometrium to the hormones of pregnancy and can mimic the appearance of an intrauterine pregnancy.
Culdocentesis
Culdocentesis may be performed to gain additional information. A needle
is inserted through the vaginal wall into the posterior culdesac. These
findings are possible:
- A dry tap is inconclusive
- A few cc's of clear fluid (peritoneal fluid) rules out a ruptured ectopic, but neither rules out nor in an unruptured ectopic.
- Slightly bloody fluid (hct <15) is inconclusive. This could be from a traumatic tap, or early, mild bleeding from an ectopic.
- Moderately bloody fluid (hct >15) indicates hemoperitoneum consistent with ruptured ectopic, but is non-specific and any internal bleeding (hemorrhagic ovarian cyst) can give this result.
- Bright red, clotting blood usually indicates a traumatic tap or aspiration of blood from a vessel.
Dilatation and curettage is sometimes done in the presence of a clearly abnormal HCG pattern, combined with abnormal ultrasound findings, to confirm or rule out ectopic pregnancy. If the D&C specimen shows chorionic villi, then the pregnancy was intrauterine. If no chorionic villi are found, then ectopic pregnancy is often presumed to be present.
Laparoscopy is a very effective method to diagnose ectopic pregnancy. Unfortunately, it is invasive, carrying its own risks, and may miss very early ectopic pregnancies that have not grown large enough to be appreciated by the operator.
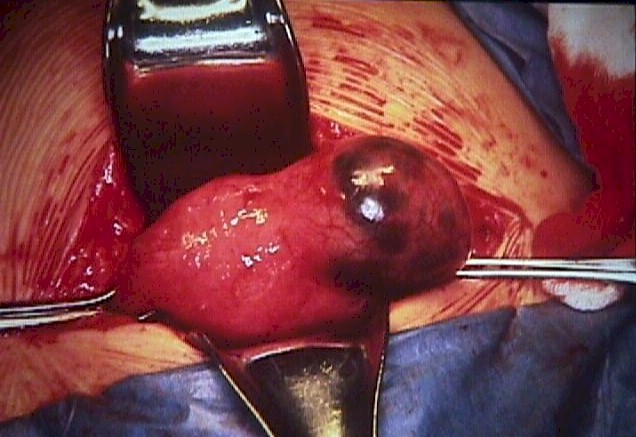
When ectopic pregnancies are found with laparoscopy, it is often possible to remove them surgically at the same time. An incision is made over the antimesenteric border of the tube and the ectopic is teased out. This can be facilitated by the injection of pitressin into the tube, causing the muscularis layer to contract, expelling the ectopic and controlling bleeding. Bleeding usually either stops or is controlled with judicious use of cautery.
Not all cases of ectopic pregnancy lend themselves to laparoscopic surgery. The larger the ectopic, the more difficult and dangerous is the laparoscopic surgery. The more bleeding that is present, the more difficult and dangerous is the laparoscopic surgery. Cornual and some isthmic ectopic pregnancies usually will need laparotomy to effectively control bleeding from the uterine side.
Laparotomy
At times, laparotomy is the best choice for dealing with an ectopic
pregnancy, particularly if the patient is bleeding heavily or is
clinically unstable.
In these cases, the priority is stopping the blood loss. The fastest and simplest way to do that is to clamp across the blood supply of the ectopic, remove it, and sew up the cut edges. This is known as a salpingectomy or partial salpingectomy, depending on the extent.
In the past, great effort was made (and considerable risk taken) to preserve childbearing potential by conserving and repairing the fallopian tube. Given the advanced state of assisted reproductive technology, such risks are only infrequently warranted today. The long-term natural fertility of a woman experiencing an ectopic pregnancy is about the same (about 50%), whether you remove the entire affected tube or try to repair it. In the event of subsequent infertility, egg retrieval, in-vitro fertilization and embryo transfer can usually leap-frog over the need for functional fallopian tubes, so immediate surgical safety and speedy recovery are usually the priorities.
Medical Management
Methotrexate is a folate antagonist originally used to treat
trophoblastic disease. It can be an effective treatment for ectopic
pregnancy.
- CBC, Platelets, Liver function tests, Renal panel
- 50 mg/sq.meter body surface area is given as a single injection. (Surface area based on a height and weight algorithm)
- Quantitative HCG day #4 and day #7
- HCG levels should fall >15% from day #4 to #7
- If HCG levels don't fall >15%, then give second dose of methotrexate
At least half of these patients will have significant abdominal pain, but the treatment will be successful in about 90% of cases in resolving the ectopic pregnancy without resorting to surgery. Some of these patients will still need surgery, either because of persistent or severe pain, hemorrhage, or failure of the HCG to resolve completely. Recovery using this method may require up to several months.
Not everyone with an ectopic pregnancy is a good candidate for this treatment. It works best when:
- The patient is compliant
- The patient prefers to avoid surgery (but with the possibility of even longer recovery from the medical treatment)
- There is desire for future childbearing
- The patient is hemodynamically stable
- The ectopic pregnancy is <3.5 cm in diameter
- There is no observable fetal cardiac activity
- There is no evidence of rupture
- HCG levels are <15,000
- There is no hepatic, renal, WBC or platelet dysfunction
Not all cases of ectopic pregnancy require surgical or medical treatment. For many ectopic pregnancies, their natural history will be to stop growing, detach and be expelled out the end of the fallopian tube, clinically disappearing.
Expectant management seems to work best when there is a plateau or falling levels of HCG , and the initial HCG is <1,000, in asymptomatic women. In such cases, successful spontaneous resolution can be expected in 75 to 90% of cases. Some of these will ultimately require methotrexate or surgery to resolve. Expectant management can be considered in other cases, but the success rate will be less. The overall successful resolution without surgery or methotrexate for ectopic pregnancies managed expectantly with initial HCG of <2000 is 60%.
Subsequent fertility has been shown to be about the same, regardless of whether the ectopic is managed expectantly, with methotrexate, or surgically.
Followup
It is important that no viable trophoblastic tissue remain following
treatment for ectopic pregnancy. For this reason, followup
HCG levels are often drawn
serially to demonstrate complete resolution of the ectopic.
Rh sensitization can occur following ectopic pregnancy treatment and Rh immune globulin is administered to Rh negative women to prevent such an event.