|
Paracervical Block |
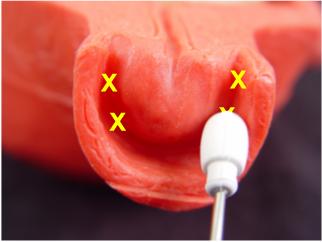
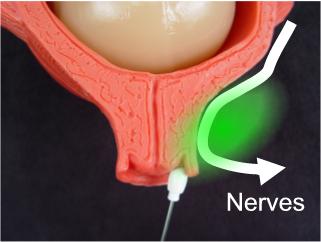 The nerves conducting the pain of labor pass next to the cervix. Blocking nerve conduction at this point blocks labor pain.
|
The pain of uterine contractions is conducted through nerves passing
close to the cervix. From there, the pain is conducted through multiple
fibers to the sympathetic chain at L2-L5.
Labor pain can be effectively blocked by interrupting the transmission of pain sensation as it passes through or close to the cervix. This is called a paracervical block. Up to 20cc of 1% Lidocaine is used. 10 cc is injected on each side of the cervix, usually in divided doses, at 10 o'clock, 8 o'clock, 2 and 4 o'clock (5 cc in each site). Usually within 5 minutes, the patient becomes completely pain free. The block will last 60-90 minutes and can be repeated. The block is effective when lidocaine reaches the broad ligament. Injections directly into the cervix may block some pain associated with dilation, it will fail to block the pain of the uterus contracting. In theory, you should be able to have a single injection site on each side of the cervix and the block will be effective. In practice, there is enough anatomic variation from person to person over the precise location of the broad ligament that experienced physicians typically will use divided doses to insure that at least some of the drug will get to where it's supposed to go. |
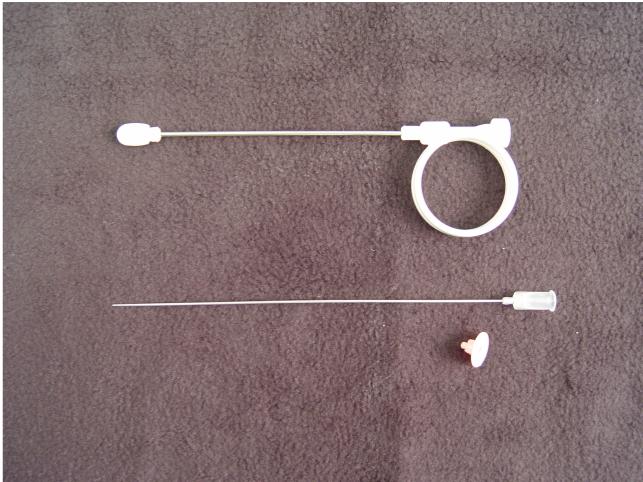
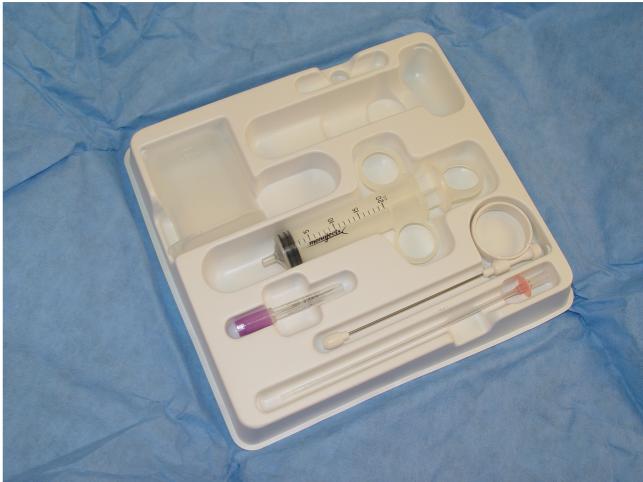 Pre-packaged Pudendal Block and Paracervical Block Set
|
How to Give a Paracervical
Block The essential equipment includes and "Iowa Trumpet," a long, hollow, blunt tube for placing at the injection site, and a matching needle, slightly longer. Pre-packaged kits typically will include both the Iowa Trumpet and the needle. Most kits will also have a plastic spacer on the needle that limits its depth of penetration to 5 mm beyond the Iowa Trumpet. Removal of the spacer allows for a full 10 mm depth of penetration (too deep for a paracervical block, but just right for a pudendal block). Open the kit and put on sterile gloves. The injection is done by feel, not by visualization. Use your right hand to examine the patient, determine the cervical dilatation, and location of the fetal presenting part. Keeping two fingers of the right hand in the vaginal, slide the Iowa Trumpet (without the needle) down the length of your vaginal fingers and direct it into the right lateral vaginal fornix. It should go in as far as it can go so the tip is resting against the vaginal mucosa of the later fornix. Adjust the Trumpet so that it is at the 8 o'clock position. Once the trumpet is in place, slide the long needle through the Iowa Trumpet until it is fully seated within the trumpet. At this point, the tip of the needle will be extending 5 mm beyond the Iowa Trumpet and just into the paracervical tissues. Aspirate to make sure you haven't perforated a blood vessel, then slowly inject 5 cc. Repeat the procedure at the 10 o'clock position. Move to the opposite side. Switch vaginal examining hands so that the left hand is in the vagina when injecting on the left side of the patient. Repeat the procedure, injecting 5 cc at 2 and 4 o'clock. |
|
Complications The only common complication from this procedure is a post-paracervical block bradycardia. This usually develops 10 to 20 minutes following injection, lasts less than 10 minutes, and resolves spontaneously. It is seen in about 10% (or less) of patients receiving paracervical blocks. The reason for the bradycardia is probably a direct fetal myocardial depressive effect of relatively high levels of fetal serum lidocaine. The base of the broad ligament is very vascular and injection of lidocaine into this area causes a relatively high, but short-lived surge in maternal lidocaine levels (below toxic levels). However, because of the acid-base gradient across the placenta (fetuses are always a little more "acidy" than their mothers) and the base nature of lidocaine, the drug is driven across the placenta, concentrating and resulting in even higher levels of lidocaine in the fetus than in the mother. Depending on the rate of absorption and the degree of acid-base gradient, the fetal lidocaine levels can reach toxic levels and have a pharmacologic effect on the fetal heart. As the lidocaine levels then rapidly fall in the mother's blood, the fetal levels also fall and the fetal heartbeat returns to baseline rates. In studies of fetal effects of this bradycardia, no change in scalp pH was measureable before, during or after the fetal bradycardia, so long as the bradycardia lasted less than 10 minutes. Rare complications, such as direct fetal injection and broad ligament hematoma have been reported. |
|
|
Patient Selection Because of the problem of potential fetal bradycardia, the paracervical block is best reserved for those patients without any significant abnormality in their fetal monitor tracing. Fetuses who already have significant variable decelerations or late decelerations will have a greater than average difference in acidity between the placenta and the mother and will be expected to be even more likely to concentrate lidocaine in their bloodstreams. Normal patients, however, have very little risk of developing a significant bradycardia that seriously threatens the fetus. |