| Delivery of the Baby |
 Delivery is also known as the second stage of labor, or part of the second
stage of labor. It begins with complete dilatation
and ends when the baby is completely out of the mother. The exact time of delivery is
normally taken at the moment the baby's anterior shoulder (the shoulder delivering closest
to the mother's pubic bone) is out.
Delivery is also known as the second stage of labor, or part of the second
stage of labor. It begins with complete dilatation
and ends when the baby is completely out of the mother. The exact time of delivery is
normally taken at the moment the baby's anterior shoulder (the shoulder delivering closest
to the mother's pubic bone) is out.
As the fetal head passes through the birth canal, it normally demonstrates, in sequence, the "cardinal movements of labor." These include:
- Engagement (fetal head reaches 0 station.)
- Descent (fetal head descends past 0 station.)
- Flexion (head is flexed with the chin to its' chest.)
- Internal Rotation (head rotates from occiput transverse to occiput anterior.)
- Extension (head extends with crowning, passing through the vulva.)
- External Rotation (head returns to its' occiput transverse orientation)
- Expulsion (shoulders and torso of the baby are delivered.)
As the fetal head descends below 0 station, the mother will perceive a sensation of pressure in the rectal area, similar to the sensation of an imminent bowel movement. At this time she will feel the urge to bear down, holding her breath and performing a Valsalva, to try to expel the baby. This is called "pushing." The maternal pushing efforts assist in speeding the delivery.
For women having their first baby, the second stage will typically take an hour or two.
Watch a video of delivery of a baby
|
|
Delivery of the baby
During the delivery, the fetal head emerges through the vaginal opening, usually facing
toward the woman's rectum.
As the fetal head delivers, support the perineum to reduce the risk of perineal laceration from uncontrolled, rapid delivery.
After the fetal head delivers, allow time for the fetal shoulders to rotate and descend through the birth canal. This pause also allows the birth canal to squeeze the fetal chest, forcing amniotic fluid out of the baby's nose and mouth.
After a reasonable pause (15-30 seconds), have the woman bear down again, delivering the shoulders and torso of the baby.
Clamp and Cut the
Umbilical Cord
After the baby is born, leave the umbilical cord alone until the baby is dried,
breathing well and starts to pink up. During this time, keep the baby more or less level
with the placenta still inside the mother.
Once the baby is breathing, put two clamps on the umbilical cord, about an inch (3 cm) from the baby's abdomen. Use scissors to cut between the clamps.
During the transition from intrauterine to extrauterine life, the umbilical cord will continue, for a short time, to provide oxygenated blood to the fetus. Once the baby is breathing, then blood is shunted to its lungs where it receives much better oxygenated blood than it was getting from the placenta.
While the cord remains intact, elevation of the fetus above the level of the placenta (for example, resting on the mother's abdomen) results in some pooling of newborn blood within the placenta and can make the baby somewhat anemic. Holding the baby below the level of the placenta results in pooling of placental blood within the newborn. This isn't good either, as the rapid homolysis of the fetal hemoglobin can lead to increased problems with neonatal jaundice. It is better to keep the baby more or less level with the placenta until the cord is clamped.
If the baby is not breathing well after delivery and needs resuscitation, immediately clamp and cut the cord so you can move the baby to the resuscitation area.
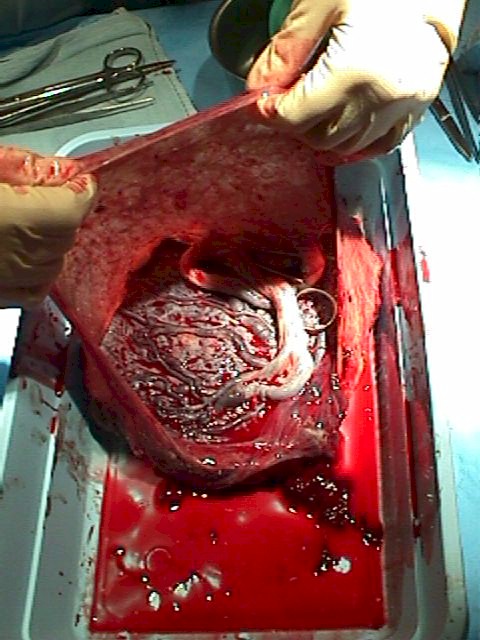
Delivery the Placenta
Immediately after delivery of the baby, the placenta is still attached inside the
uterus. Some time later, the placenta will detach from the uterus and then be
expelled. This process is called the "3rd stage of labor" and may take just a
few minutes or as long as an hour.
Signs that the placenta is beginning to separate include:
- A sudden gush of blood
- Lengthening of the visible portion of the umbilical cord.
- The uterus, which is usually soft and flat immediately after delivery, becomes round and firm.
- The uterus, the top of which is usually about half-way between the pubic bone and the umbilicus, seems to enlarge and approach the umbilicus.
Immediately after the delivery of the baby, uterine contractions stop and labor pains go away. As the placenta separates, the woman will again feel painful uterine cramps. As the placenta descends through the birth canal, she will again feel the urge to bear down and will push out the placenta.
If the placenta is not promptly expelled, or if the patient hemorrhages while awaiting delivery of the placenta, this is called a "retained placenta" and it should be manually removed.
After delivery of the placenta, the uterus normally contracts firmly, closing off the open blood vessels which previously supplied the placenta. Without this contraction, rapid blood loss would likely prove very problematic or worse.
To encourage the uterus to firmly contract, oxytocin 10 mIU IM can be given after delivery. Alternatively, oxytocin 10 or 20 units in a liter of IV fluids can be run briskly (150 cc/hour) into a vein. Breast feeding the baby or providing nipple stimulation (rolling the nipple between thumb and forefinger) will cause the mother's pituitary gland to release oxytocin internally, causing similar, but usually milder effects.
A simple way to encourage firm uterine contraction is with uterine massage. The fundus of the uterus (top portion) is vigorously massaged to keep it the consistency of a tightened thigh muscle. If it is flabby, the patient will likely continue to bleed.